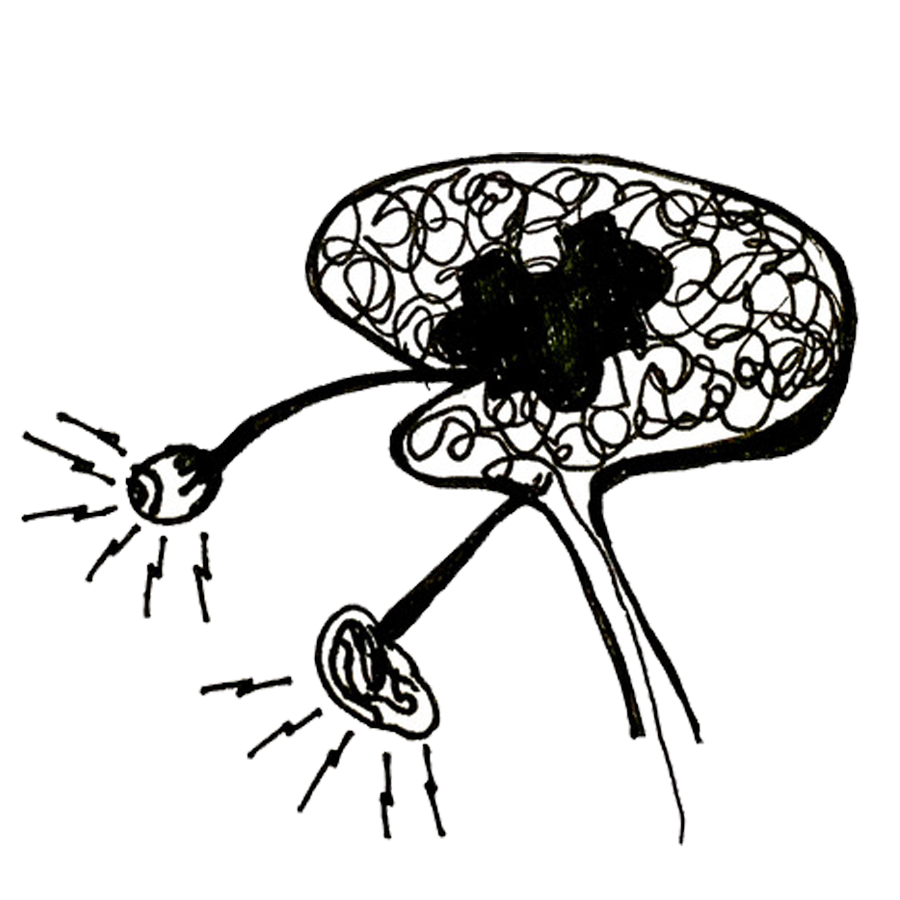
Sensory overload

For the last three years, Covid long haulers have had to become their own advocates and researchers as they lobby for recognition, funding and proper healthcare. Their knowledge has been hard-won against a backdrop of sickness. They’ve pushed through symptoms that ravaged their previously able-bodies and become the experts of their own disease.
That is why we decided that all the symptoms on this website should be written by patients, for patients. As our co-founder Jenene Crossan says “They poured their hearts, their souls and their deep determination to find just enough energy to put their experiences down for others to benefit from”.
Although we do not intend to give medical advice, the articles have been fact-checked by a wonderful doctor who is suffering from Long Covid too.
About the author
I previously worked full time in a demanding career that I loved. I was reasonably fit, in my mid-late 40s and had a medically managed autoimmune disease. Life was busy, with a mixture of people interactions and computer work, parenting, and running a household. Since catching Covid-19 in April 2022 and developing Long Covid, I suffer from frequent sensory overload – particularly from noise, light and movement.
– Female, NZ European, Central Otago

DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
Content shared on this website is for informational purposes only. It should not be taken as a substitute for professional medical advice. Always seek the advice of a qualified healthcare professional regarding a medical condition, diagnosis or possible treatments. Long Covid Support Aotearoa is not liable for risks associated with using or acting upon the information provided on this website.