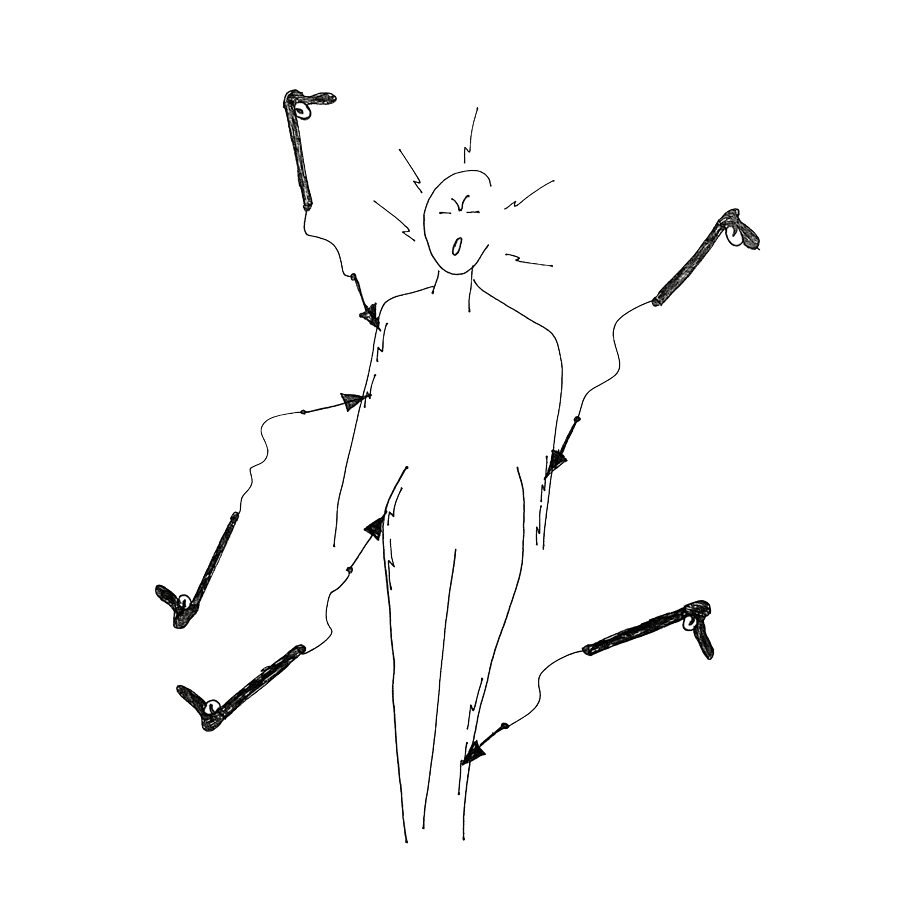
Nerve pain

For the last three years, Covid long haulers have had to become their own advocates and researchers as they lobby for recognition, funding and proper healthcare. Their knowledge has been hard-won against a backdrop of sickness. They’ve pushed through symptoms that ravaged their previously able-bodies and become the experts of their own disease.
That is why we decided that all the symptoms on this website should be written by patients, for patients. As our co-founder Jenene Crossan says “They poured their hearts, their souls and their deep determination to find just enough energy to put their experiences down for others to benefit from”.
Although we do not intend to give medical advice, the articles have been fact-checked by a wonderful doctor who is suffering from Long Covid too.
About the author
I was learning to live with Post-treatment Lyme Disease Syndrome (PTLDS) when I caught Covid at the very beginning of the pandemic. It was February 2020 and I was in my mid-30s, living in Canada. My symptoms were a high spiking fever, shortness of breath, a sore throat, intense fatigue and brain fog. I could barely stand and began fainting – once, for eight hours as I waited in an emergency room. Staff were overwhelmed and confused, and sent me home.
After three months with Lyme disease, I could walk, dance and mahi | work in hospitality, even if I was in a bit of pain. But once I got Covid, everything became so much worse. I only ever managed to walk a kilometre before fatigue would strike. Brain fog would kick in if I read or worked for more than an hour. I developed fibromyalgia and nerve pain, Chronic Fatigue Syndrome, viral arthritis, irritable bowel syndrome, acid reflux, hair loss… every month, it was something new.
It’s taken three years and a lot of work to slowly recover to who I am today. First, I had to accept that I was now disabled and mourn the loss of who I was. Then to accept this new person and learn who the new ‘me’ is. The last step was to learn to manage my life. It’s an all-consuming task and it all adds up: what I eat, how much I mahi work, how much I walk or swim, how I whakatā | rest afterwards.
This effort and an 18-month regime of herbal supplements has helped to slowly move the needle for me. I’m finally able to swim, walk more and dance, but always with careful planning and pain-management tools. The pain in my muscles and nerves never goes away, and leads to intense brain fog if I can’t moderate my days.
– Non-binary, Indian, Pōneke/Wellington

DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
Content shared on this website is for informational purposes only. It should not be taken as a substitute for professional medical advice. Always seek the advice of a qualified healthcare professional regarding a medical condition, diagnosis or possible treatments. Long Covid Support Aotearoa is not liable for risks associated with using or acting upon the information provided on this website.