Insomnia

For the last three years, Covid long haulers have had to become their own advocates and researchers as they lobby for recognition, funding and proper healthcare. Their knowledge has been hard-won against a backdrop of sickness. They’ve pushed through symptoms that ravaged their previously able-bodies and become the experts of their own disease.
That is why we decided that all the symptoms on this website should be written by patients, for patients. As our co-founder Jenene Crossan says “They poured their hearts, their souls and their deep determination to find just enough energy to put their experiences down for others to benefit from”.
Although we do not intend to give medical advice, the articles have been fact-checked by a wonderful doctor who is suffering from Long Covid too.
About the author
Before I caught Covid-19 in March 2022, I was very fit and active. I walked every day, attended dance classes every week and ran my own business while also looking after three tamariki | children.
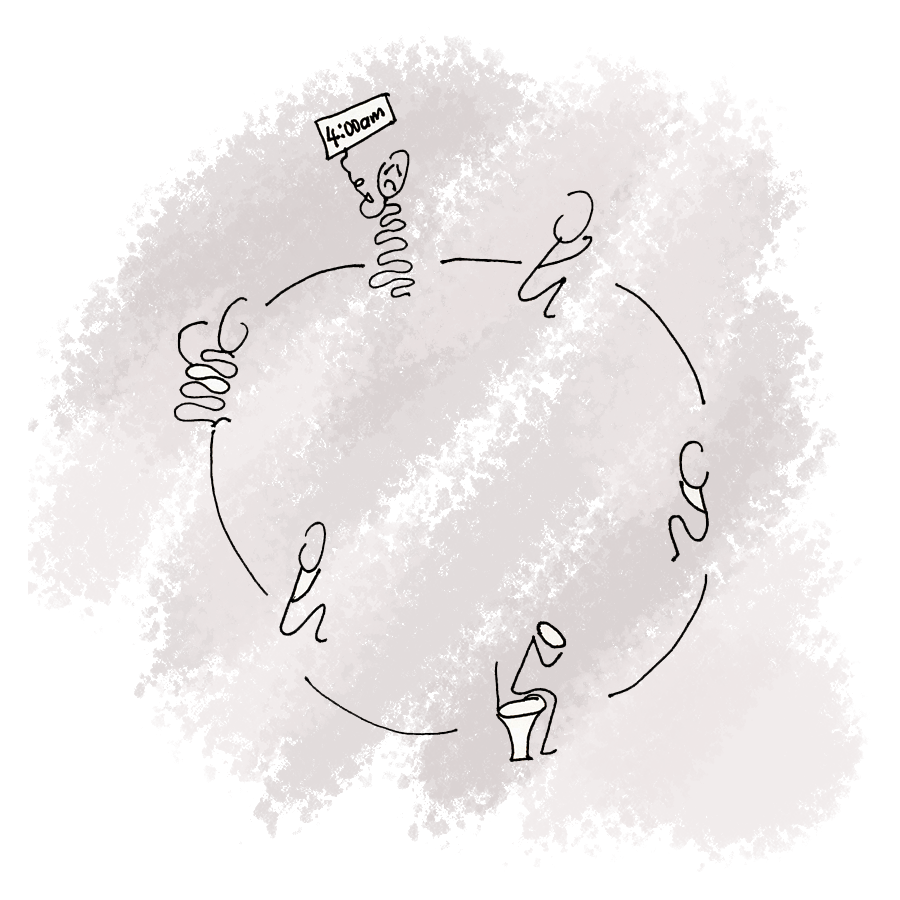
When I got the virus in my early 50s, my health took a major hit. As well as breathlessness, fatigue and heart issues, I had difficulty sleeping, and asked my doctor for āwhina | help with this. Ten months after my infection, my moe | sleep has thankfully improved lots – but if I overdo it, symptoms can quickly return.
– Non-binary, European, Pōneke/Wellington